Health
Support for individuals harmed by Covid vaccines under scrutiny
Those who have experienced rare blood clots are expressing feelings of being overlooked amidst the pandemic.
The existence of risk is inherent in all aspects of life, including vaccination. Nevertheless, the available evidence suggests that the benefits of vaccination with recommended vaccines in the UK significantly outweigh the potential for severe side effects.

The benefits of Covid-19 vaccines have been extensively documented, with the Oxford/AstraZeneca vaccine credited with saving approximately 6.3 million lives worldwide in its first year of use, surpassing the 5.9 million lives saved by the Pfizer/BioNTech vaccine.
While Covid-19 vaccines have had a profoundly positive impact, it is also essential to acknowledge the experiences of individuals who have suffered adverse effects, including those affected by the AstraZeneca vaccine.
Around 50 families who have been impacted by rare blood clots are pursuing a group legal action under the Consumer Protection Act, arguing that the vaccine did not meet the expected safety standards.
These families include individuals who have experienced severe physical harm, are unable to work, and those who have lost loved ones due to vaccine-related injuries.
Although these cases represent a small fraction of the total number of vaccinated individuals, the impact on the affected families is significant, and they feel that their concerns have been overlooked.
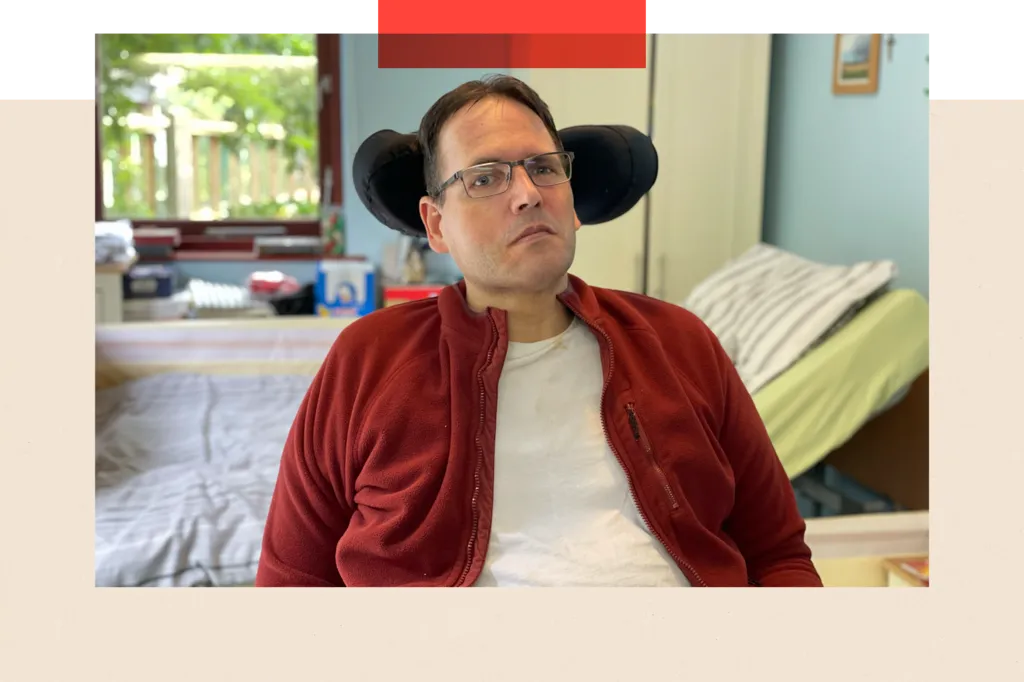
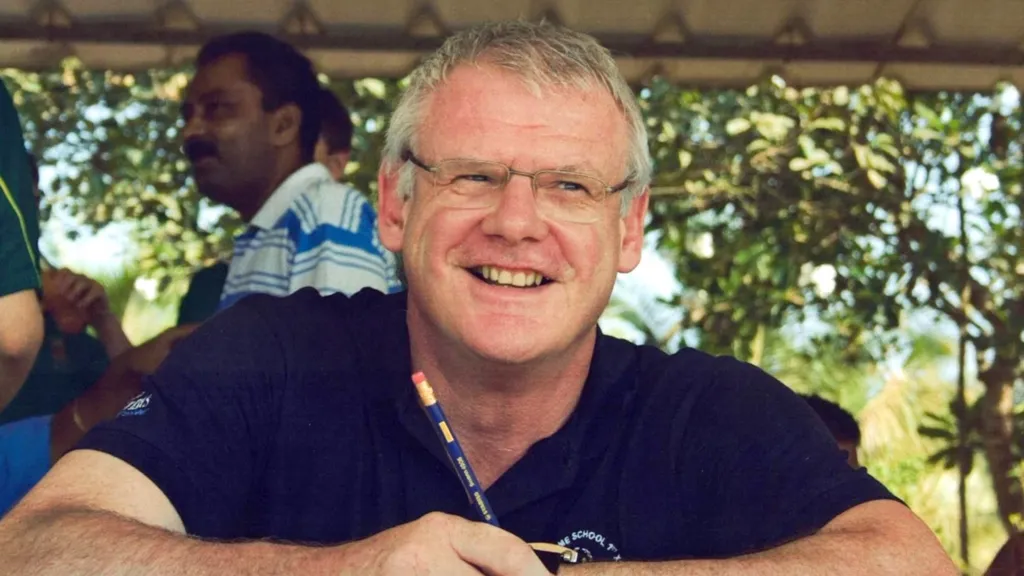
One such family is that of Jane and Ian Wrigley from Buckinghamshire, who have been significantly affected by the vaccine.
Prior to receiving the vaccine, Jane, 62, was an active individual who enjoyed running, skiing, and climbing; however, she is now severely weakened on her left side and struggles to walk.
Two weeks after receiving the AstraZeneca vaccine in March 2021, Jane was hospitalized due to blood clots in her brain, which required emergency surgery to remove a portion of her skull; her medical records confirm that the vaccine was the cause of these clots.

Ian now serves as Jane's full-time caregiver, and Jane has expressed that she has lost her independence, having previously been an active and independent individual.
The cases of individuals like Jane, who have experienced severe side effects from the vaccine, raise concerns about the support system in place for those who have suffered harm as a result of Covid-19 vaccination.
In 2021, nearly 25 million adults in the UK received the first dose of the Oxford/AstraZeneca vaccine, with the majority also receiving a second dose.
The Covid-19 vaccine program is estimated to have prevented over 250,000 hospital admissions and more than 120,000 deaths in the UK by September 2021.
Typically, vaccine side effects are mild and short-term, such as arm soreness, fever, and fatigue.
However, in rare instances where severe adverse effects occur, individuals have the right to expect support, which is a fundamental aspect of the social contract between individuals and the state.
The Vaccine Damage Payment Scheme (VDPS) was established in 1979 to address concerns about vaccine safety, particularly regarding the whooping cough vaccine.
The government-backed VDPS provides a one-time payment of £120,000 to individuals who have suffered at least 60% disability as a result of vaccination, as determined by the balance of probability.
Between the late 1970s and 2020, there were approximately 6,500 claims under the VDPS for all vaccines, resulting in 944 awards.
The Covid-19 pandemic has led to a significant increase in claims under the VDPS, with many individuals seeking compensation for vaccine-related injuries.

The Oxford/AstraZeneca vaccine has been credited with saving millions of lives, but it has also been associated with rare and severe side effects, including blood clots in the brain, which can be fatal.
A documentary exploring the stories of individuals affected by Covid-19 vaccines is available to watch.
Since the pandemic, there has been a substantial increase in VDPS claims, with over 16,000 claims filed against Covid-19 vaccines, resulting in 180 awards, and more than half of claimants still awaiting a decision.
The majority of awards have been for damage caused by the AstraZeneca Covid-19 vaccine, which is no longer in use.
A specific rare side effect associated with the AstraZeneca vaccine, characterized by blood clots and low platelet levels, has been identified as a qualifying condition for VDPS payments.
This side effect, known as vaccine-induced thrombosis with thrombocytopenia (VITT), was not observed in clinical trials but emerged after the vaccine was administered to millions of people.
VITT is a rare condition that can cause damage to the brain and other organs, typically occurring within a few weeks of receiving the first dose of the vaccine.
The combination of blood clots and low platelet levels is unusual, prompting experts to coin the term VITT to describe this specific condition.
Although clinical trials involving over 23,000 participants did not detect this signal, it became apparent once the vaccine was widely administered across Europe.
In response to concerns about the blood clot link, several European countries temporarily suspended use of the AstraZeneca vaccine in mid-March 2021.
The UK restricted the use of the vaccine to individuals over 30 years old in April 2021 and later to those over 40, as it became clear that younger people were at higher risk of experiencing blood clots.
Other European countries also imposed age restrictions on the vaccine, with some countries limiting its use to individuals over 55 or 60 years old, while Denmark halted its use entirely.
By early April 2021, regulatory agencies in the UK and Europe had concluded that blood clots combined with low platelet levels should be listed as a rare side effect of the vaccine.
A similar rare syndrome has been reported in recipients of the J&J Janssen Covid-19 vaccine in the United States, which uses similar vaccine technology.
According to Sarah Moore, a solicitor with Leigh Day, the families she represents are seeking legal action against AstraZeneca due to the inadequacies of the VDPS.
Moore criticizes the VDPS, stating that it provides insufficient support to too few individuals, with the £120,000 payment being "woefully inadequate" and not having increased since 2007.
If the payment had kept pace with inflation, it would now be approximately £197,000.
Moore's clients include individuals who require 24-hour care, are unable to perform daily tasks, and have suffered severe physical or cognitive impairments, rendering them unable to work again.
The case of Jane and Ian Wrigley highlights another criticism of the VDPS: delays in the payment process.
The couple waited over two years for a payment under the scheme, despite a clear link between the vaccine and Jane's condition, with assessments being conducted on paper without physical examinations.
In response to criticisms, the government has announced efforts to modernize the VDPS, increasing the number of staff handling claims from four to 80, but a significant backlog of claims remains.
Among those affected by the AstraZeneca vaccine is Peter Schulze, a 49-year-old who developed VITT blood clots after receiving the vaccine in April 2021. As a result, he now requires constant care.
Schulze submitted his claim to the VDPS in July 2022, but a decision has yet to be made, despite clear evidence of VITT blood clots in his medical records.
A significant hurdle for claimants is the 60% disablement threshold, which has disqualified numerous individuals who have been officially recognized as suffering from Covid vaccine-related damage.
According to Ms Moore, one of her clients, a woman who is now blind in one eye and suffers from other physical and psychological injuries, was informed that her condition did not meet the 60% threshold.
Under standard civil claim rules, blindness in one eye could result in compensation exceeding £200,000, making it particularly distressing for individuals to be told they do not qualify for payment despite suffering vaccine-related injuries.
During the pandemic, the government granted vaccine manufacturers, including AstraZeneca, legal indemnity, which determined the party responsible for paying compensation in the event of a successful claim.
Then-Health Secretary Matt Hancock stated in the Commons that the government was providing indemnities to cover any unforeseen adverse reactions, despite the robust checks and procedures in place.
Ms Moore believes that this indemnity means the government will cover AstraZeneca's legal costs and be liable for compensation payments if a claim is successful, although she has not seen the relevant documents.
AstraZeneca did not profit from its Covid vaccine, Vaxrevia, but the company's total revenue in 2023 was $45.8bn (£35.1bn), with profits of $5.9bn.
In May, AstraZeneca discontinued Vaxrevia, citing an surplus of updated vaccines, and the UK government did not purchase any doses for its booster programs, instead opting for Pfizer and Moderna vaccines, which utilize mRNA technology.
Prof Adam Finn, a leading expert on vaccines and former member of the JCVI, played a key role in advising the government on immunization policies during the pandemic.
Prof Finn was involved in crucial decisions regarding the rollout of Covid vaccines, including the order in which they were administered and the age restrictions imposed on the AstraZeneca vaccine due to blood clot risks.
While not involved in the current legal action, Prof Finn believes that the decisions made regarding Covid vaccine use in the UK were correct and that the vaccines have been highly effective in saving lives.
However, he expresses concerns that the VDPS is not functioning as intended and suggests that payments should be index-linked to reflect changes in the cost of living, while also criticizing the 60% threshold as arbitrary.
Prof Finn advocates for a thorough review of compensation for current and future vaccines, emphasizing the need for a fair and effective system.
When asked about the potential impact of this report on vaccine confidence, Prof Finn emphasizes the importance of honesty and transparency in maintaining public trust.
He warns that the inadequacies of the VDPS could erode public confidence in vaccines, which is crucial for their effectiveness.
Although the number of people affected by vaccine-related injuries is relatively small, the severity of their harm will attract public attention and raise questions about fair treatment.
AstraZeneca has issued a statement expressing sympathy for those who have experienced health problems or lost loved ones, while also emphasizing the safety profile of its vaccine.
The company's statement notes that regulators worldwide have consistently stated that the benefits of vaccination outweigh the risks of rare potential side effects.
Recently, Health Secretary Wes Streeting met with individuals who have been injured or bereaved due to vaccine damage, in an effort to listen to their concerns.
The Department of Health and Social Care has stated that the government will carefully consider these concerns as it continues to learn from the pandemic.
The department has expressed its deepest sympathies to those who have suffered harm and is working to address the issues raised.
The VDPS administrator has implemented operational changes to reduce the waiting time for claimants, in an effort to improve the efficiency of the scheme.
The Covid inquiry, which will begin taking evidence in January 2025, will examine the workings of the VDPS in its next module.
Ms Moore, who is expected to give evidence to the inquiry, emphasizes that her clients are not opposed to vaccination, but rather seek support and fairness for those who have been affected by vaccine-related injuries.
She stresses that her clients are, by definition, pro-vaccination, having chosen to get vaccinated, and that their goal is to promote vaccine confidence through fair compensation.
The legal action against AstraZeneca is likely to be a prolonged process, with no immediate resolution in sight.
Additional research for this report was conducted by Catherine Snowdon.
Health
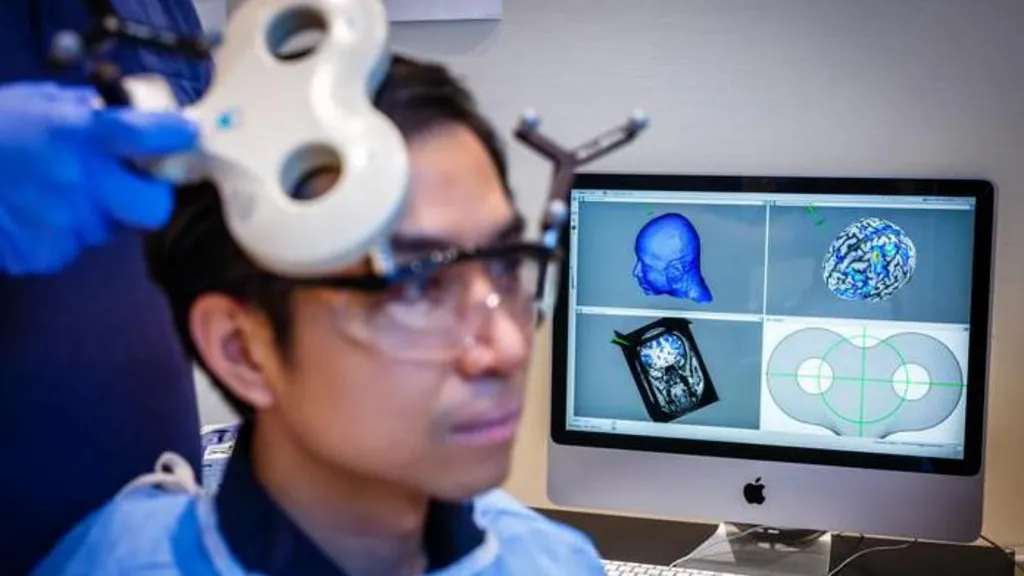
Study Explores if Brain Stimulation Can Reduce Selfish Behavior
Researchers have found a way to temporarily and marginally decrease self-centered behavior in individuals by activating two specific regions of the brain.
Researchers have made a groundbreaking discovery, finding that temporary reductions in selfish behavior can be achieved by stimulating specific areas of the brain.
A recent study conducted at the University of Zurich involved 44 participants who were tasked with dividing a sum of money between themselves and an anonymous partner, allowing scientists to observe their decision-making processes.
The experiment utilized electrical current to stimulate the frontal and parietal regions of the brain, located at the front and rear of the skull, respectively. When these areas were stimulated simultaneously, participants exhibited a greater willingness to share their funds.
According to Prof Christian Ruff, a lead author of the study, the observed effects were consistent, albeit modest in scale.
Statistical analysis revealed a notable increase in participants' willingness to allocate funds to others, indicating a shift in their behavior.
The findings not only provide insight into the neural mechanisms underlying fundamental human behavior but may also have implications for the treatment of certain brain disorders characterized by impaired social behavior.
Prof Ruff noted that some individuals struggle with profound social difficulties due to an inability to consider others' perspectives, leading to consistently selfish behavior, and suggested that this discovery could potentially be used to address such issues.
However, the effects of the brain stimulation were found to be short-lived, suggesting that repeated application may be necessary to achieve lasting changes.
Prof Ruff likened the potential effects of repeated stimulation to the benefits of regular exercise, stating that consistent application over a prolonged period could lead to significant changes in behavior, much like the physical adaptations that occur with regular gym attendance.
This latest discovery builds upon a previous study in which researchers monitored brain activity while participants engaged in a similar money-sharing game, providing a foundation for the current findings.
The earlier study identified two brain regions that appeared to be synchronized, with neural activity occurring at the same frequency, when participants made more generous decisions.
These brain areas are known to play a crucial role in decision-making and empathy, enabling individuals to distinguish between their own feelings and those of others.
When participants made selfless decisions, the regions responsible for empathy and decision-making were found to be communicating with each other.
The researchers sought to investigate whether electrical stimulation could be used to influence this communication and promote more selfless decision-making.
One participant who underwent the brain stimulation test described the experience as a gentle, soothing sensation, comparable to a warm shower or light rain on the scalp.
The participant reported making decisions while receiving the stimulation without feeling any external influence on their choices.
The discovery of a consistent neural pattern associated with selfless decision-making across multiple individuals suggests that altruism may be an innate, evolutionarily conserved trait that enables humans to care for one another.
Prof Ruff emphasized the clinical significance of this finding, highlighting the potential to modify and influence this neural mechanism.
Dr Jie Hu, a co-author of the study, noted that the research provides evidence of a causal relationship between brain activity and decision-making, demonstrating that targeted stimulation can alter an individual's sharing behavior.
By manipulating communication within a specific brain network using non-invasive stimulation, the researchers observed a shift in participants' decisions, influencing the balance between self-interest and altruism.
Addressing concerns about the potential implications of this research, Prof Ruff assured that the experiment was conducted with strict adherence to medical regulations and ethical guidelines, ensuring the well-being and informed consent of all participants.
The neuroscientist drew a distinction between the controlled, medically regulated nature of the experiment and the often-subliminal influences of social media and advertising, which can affect behavior without explicit consent.
Prof Ruff suggested that, in contrast to the experiment, the impacts of social media and advertising on brain function and behavior are often unforeseen and uncontrolled, highlighting the importance of careful consideration and regulation in such contexts.
Health
NHS Workers to Receive 3.3% Pay Increase
Labor unions have expressed displeasure, yet the government maintains that its actions showcase a dedication to its workforce.
The government has confirmed that NHS staff in England will receive a 3.3% pay increase in the upcoming financial year.

This pay award applies to approximately 1.4 million health workers, including nurses, midwives, physiotherapists, and porters, but excludes doctors, dentists, and senior management.
Although the Department of Health and Social Care initially proposed a lower figure, it has accepted the recommendation of the independent pay review body to demonstrate its commitment to NHS staff, resulting in a higher pay rise than initially suggested.
However, several health unions have expressed disappointment with the announced pay award.
Prof Nicola Ranger, general secretary of the Royal College of Nursing (RCN), noted that the 3.3% increase falls short of the current consumer price index (CPI) inflation rate of 3.4%, which measures the rise in prices over the past year.
Prof Ranger stated, "A pay award that is lower than the current inflation rate is unacceptable, and unless inflation decreases, the government will be imposing a real pay cut on NHS workers."
She criticized the government's approach, saying, "This strategy of making last-minute decisions is not an appropriate way to treat individuals who are essential to a system in crisis."
Prof Ranger indicated that she would wait to see the pay awards for the rest of the public sector and doctors before deciding on a course of action.
The RCN had previously reacted strongly to the 5.4% pay increase received by resident doctors last year, compared to the 3.6% increase received by nurses, which they described as "grotesque".
Prof Ranger emphasized, "Nursing staff will not accept being treated with disrespect, as has happened in the past when they were given lower pay awards than other groups."
Helga Pile, head of health at Unison, the largest health union, commented, "NHS staff who are already under financial pressure will be outraged by another pay award that fails to keep up with inflation."
"Once again, they are expected to deliver more while their pay effectively decreases, as it falls behind the rising cost of living," she added.
In response, the government argued that the pay award is actually above the forecasted inflation rate for the coming year, which is around 2%.
A spokesperson for the Department of Health and Social Care stated, "This government greatly values the outstanding work of NHS staff and is committed to supporting them."
The pay increase is expected to be implemented by the start of April.
However, the government did not provide a timeline for the announcement on doctors' pay, as the pay review body responsible for making recommendations on their pay has yet to submit its report to ministers.
The government is currently engaged in negotiations with the British Medical Association regarding the pay of resident doctors, previously known as junior doctors.
Members of the BMA recently voted in favor of strike action, granting them a six-month mandate for walkouts, and there have been 14 strikes so far in the ongoing dispute.
Health
NHS Waiting List Hits Three-Year Low
In England, the backlog has fallen below 7.3 million for the first time since 2023, yet worries persist regarding prolonged waiting times in accident and emergency departments.
England's hospital waiting list has reached its lowest point in almost three years, marking a significant milestone in the country's healthcare system.

As of December 2025, the number of patients awaiting treatment, including knee and hip operations, stood at 7.29 million, the lowest figure recorded since February 2023.
However, the latest monthly update from NHS England reveals that long wait times persist in Accident and Emergency departments, with a record number of patients experiencing 12-hour trolley waits.
In January 2026, over 71,500 patients spent more than 12 hours waiting for a hospital bed after being assessed by A&E staff, the highest number tracked since 2010.
This translates to nearly one in five patients admitted after visiting A&E waiting for an extended period.
According to Health Secretary Wes Streeting, while progress has been made, significant challenges still need to be addressed.
Streeting acknowledged that "there is much more to do" and emphasized the need to accelerate progress, but expressed optimism that the NHS is on the path to recovery.
Dr. Vicky Price, representing the Society for Acute Medicine, noted that hospitals are operating beyond safe capacity in terms of emergency care.
Dr. Price highlighted the vulnerability of patients who require admission, often elderly and frail individuals with complex needs, who are at greater risk of harm when care is delivered in corridors and hospitals exceed safe limits.
Duncan Burton, Chief Nursing Officer for England, commended the progress made in reducing wait times, achieved despite the challenges posed by strikes by resident doctors.
Burton attributed this progress to the hard work and dedication of NHS staff, describing it as a "triumph".
Although the waiting list decreased, performance against the 18-week target slightly declined, with 61.5% of patients waiting less than 18 weeks, compared to 61.8% in November, and still short of the 92% target set to be met by 2029.
Rory Deighton of the NHS Confederation, which represents hospitals, welcomed the progress but cautioned that it obscures significant regional variations.
A recent BBC report revealed that nearly a quarter of hospital trusts experienced worsening wait times over the past year.
Deighton emphasized that the NHS is composed of numerous separate organizations, each with unique financial and operational challenges, making it more difficult to address care backlogs in some areas.
According to Deighton, this means that tackling care backlogs will be more challenging in certain parts of the country due to these distinct regional challenges.
-

 News8 hours ago
News8 hours agoAustralian Politics Faces Questions Over Gender Equality Amid Sussan Ley’s Appointment
-
 News5 hours ago
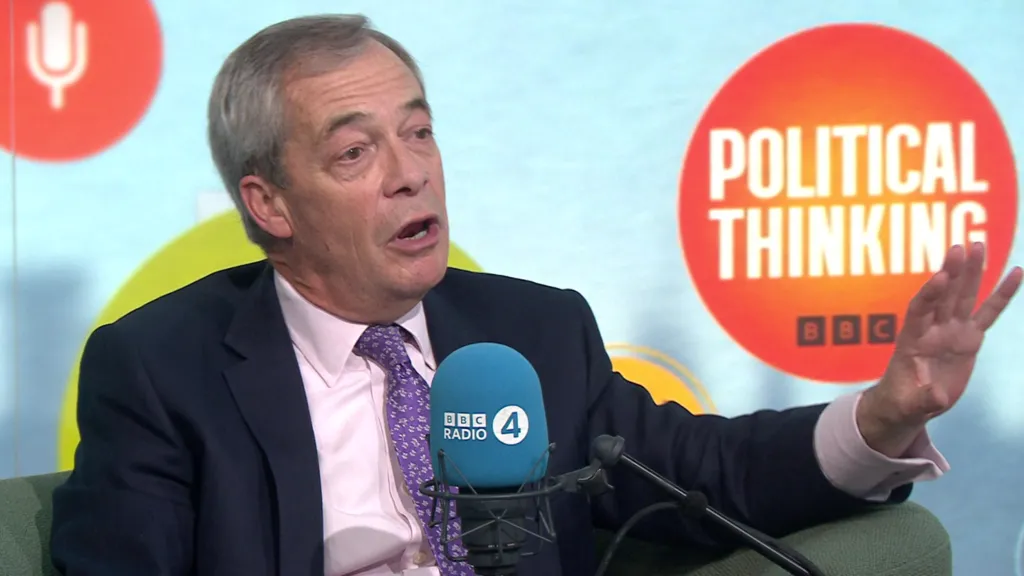
News5 hours agoFarage Says Reform to Replace Traditional Tory Party
-

 News5 hours ago
News5 hours agoWrexham Pair Seek Win Against Former Team Ipswich
-

 News11 hours ago
News11 hours agoLiberal Party Removes Australia’s First Female Leader
-

 News9 hours ago
News9 hours agoUK Braces for Cold Snap with Snow and Ice Alerts Expected
-
 News5 hours ago
News5 hours agoHusband’s alleged £600k theft for sex and antiques blamed on drug side effects
-

 News2 days ago
News2 days agoSunbed ads spreading harmful misinformation to young people
-

 Business11 hours ago
Business11 hours agoBBC Reporter Exposed to Cyber Attack Due to Vulnerabilities in AI Coding Tool